"Midwifery, I believe, is the answer - to put a well-trained midwife in every village would soon eradicate obstetric fistula."
- Dr Catherine Hamlin
Most New Zealand women would never imagine giving birth without a midwife or doctor present. Yet for 70% of rural Ethiopian women, this is their reality. Not only is there often no medical help available, but that help can be a two-day walk away. Challenged by its rugged terrain and developing infrastructure, Ethiopia has made enormous progress in reducing their maternal mortality rate by 70% since 1990. The Hamlin midwives are setting the standard for care in pregnancy and childbirth in Ethiopia, and we need more of these highly trained professionals to combat the risks of unsupported labour to mother and baby.


One of the worst things that can happen to a woman is an obstetric fistula, an internal injury caused by a prolonged obstructed labour during childbirth that leaves her incontinent and humiliated with a horrible lingering odour. In the majority of cases, the baby is tragically born stillborn.
To really prevent fistula requires one main thing – the education and deployment of midwives, making quality maternity care accessible for every woman in Ethiopia.
From the beginning, Dr Reg and Dr Catherine dreamed of training midwives as part of the program of prevention throughout Ethiopia. Catherine opened the Hamlin College of Midwives in 2007. Since then, over 230 Hamlin Midwives have graduated and are making a significant impact in rural communities, drastically reducing rates of fistula and providing quality maternal health care.
The Hamlin College of Midwives recruits students from rural areas, puts them through rigorous training as midwives, and deploys them back to their villages where their skills are needed. There are another 95 women currently completing their Bachelor of Science in Midwifery degree at the College.
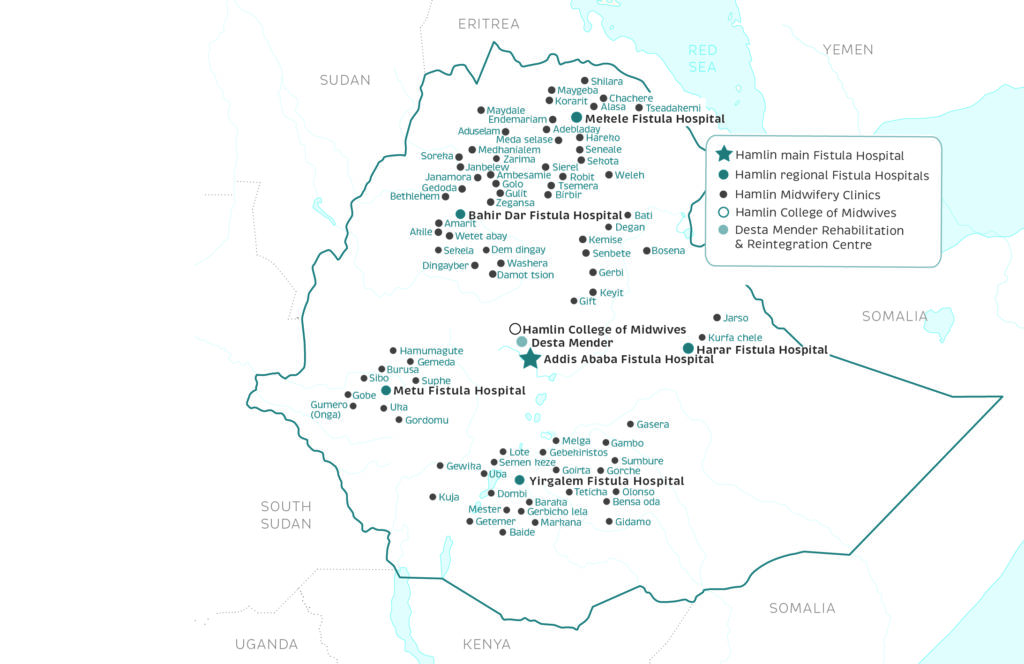
Providing funding support towards fistula prevention is the primary priority for Hamlin Fistula New Zealand. There are now 92 Hamlin-supported midwifery clinics in rural health centres staffed by Hamlin midwives. The downstream effects of a Hamlin midwife are remarkable; when a Hamlin midwife arrives, new cases of fistula drop to almost zero in nearby villages. These centres are key to prevention.
Hamlin Fistula New Zealand’s focus is on preventing fistula through increasing the number of dedicated midwifery centres and training of skilled midwives.
The introduction of a master’s postgraduate course in clinical midwifery course, launched in January 2022, is equipping senior midwives with advanced clinical practice skills, including the skills to perform emergency caesarean deliveries for complicated cases. This will empower midwives in preventing maternal death and injury among vulnerable rurally based women, who are unable to make the journey to a Hamlin Hospital.
Equip a young midwife with a scholarship

In partnering with us you can make a life-saving impact for thousands of vulnerable women and babies.